OPERATIONS & ADMIN
Manage 100 or 10,000 Patients with the Same Team
One operating system for APCM, RPM, CCM, and RTM—from eligibility and onboarding to billing, compliance, and scale.
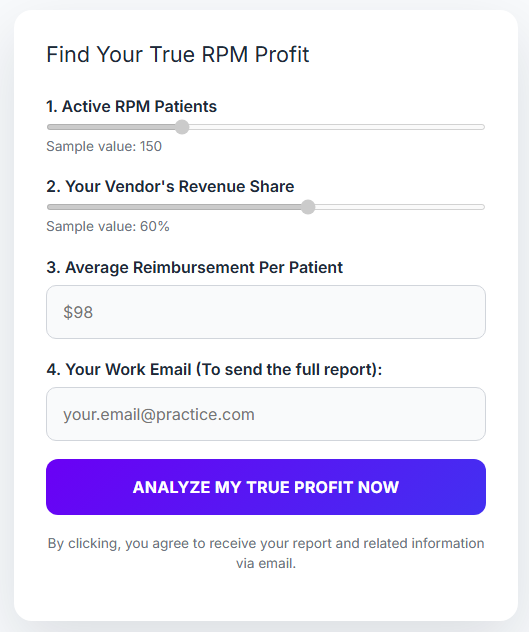
The most common objection to bringing RPM, APCM, RTM, or CCM in-house is bandwidth. FairPath’s queue-based architecture lets you work as little or as much as you want: whether you have 30 minutes a day or a dedicated team, the system prioritizes work so you never waste time, eliminate repetitive manual steps, and keep the focus on patient health first.
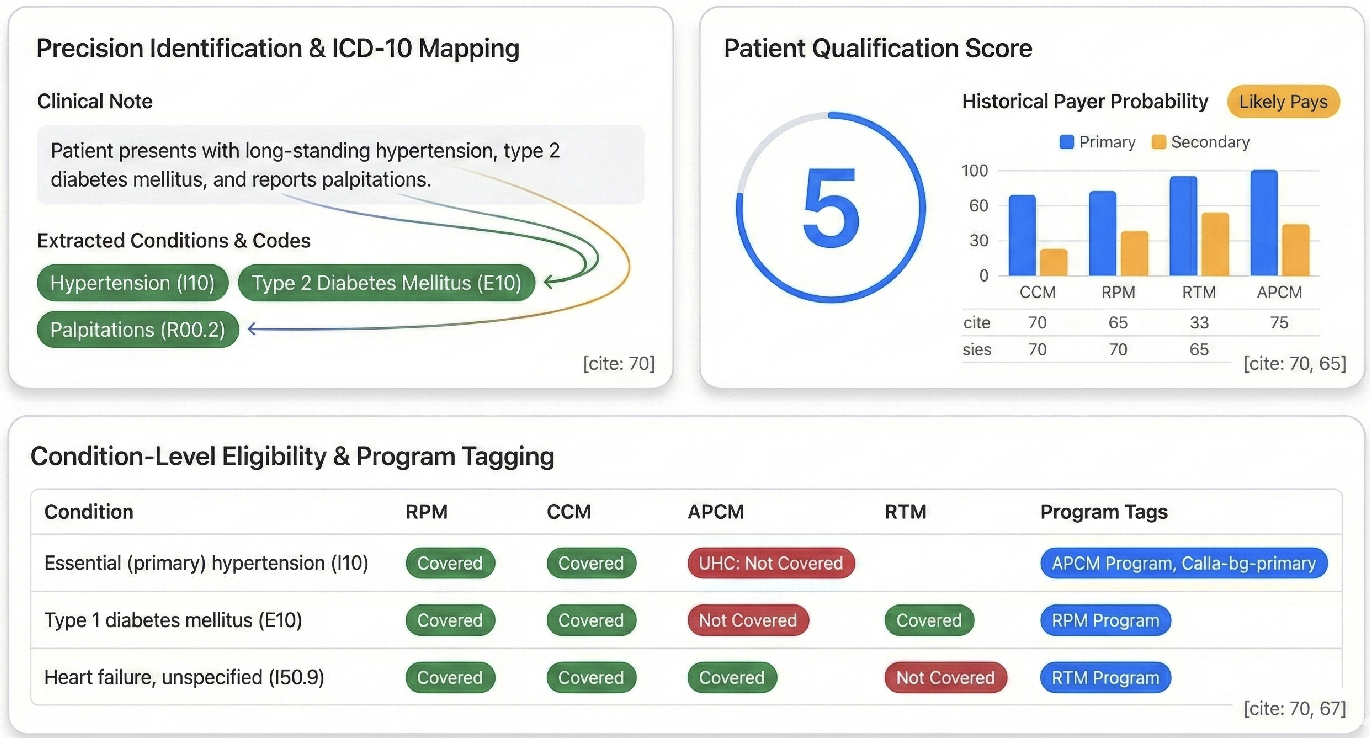
Eligibility & Panel Design: Stop Guessing, Start Targeting
Most practices struggle with remote care because they improvise who to enroll. FairPath replaces guesswork with structured, scalable decision-making. We turn the chaos of payer rules, diagnosis codes, and payment history into a single 1–5 Qualification Score for each patient, so you see exactly who is viable for APCM, RPM, CCM, or RTM without manual chart review.
ERA & Payment Intelligence
Predictive payer scoring built from your own data. FairPath ingests your 835 (ERA) payment files to learn from your actual claims history, predicting which payers and codes will reimburse and filtering out high-denial plans before you ever start enrollment.
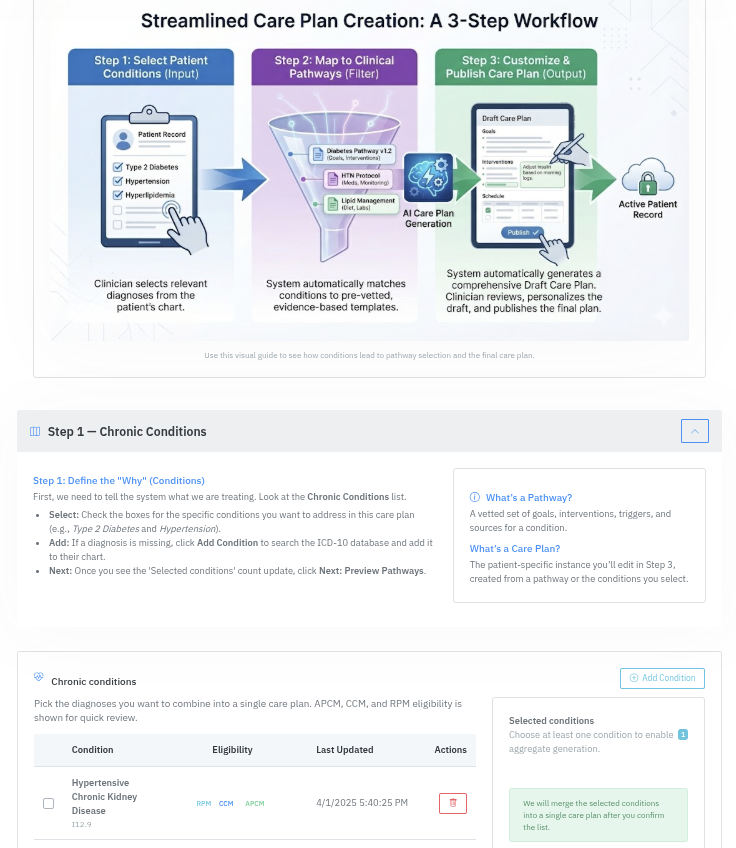
Condition-Level Mapping
One dashboard maps diagnoses to programs (e.g., HTN, Diabetes, COPD, CKD → APCM, RPM, CCM), showing which chronic conditions qualify for which programs in a single, simple table tuned to your clinical policies.
Always-Current Rules Engine
We automatically update the logic for CMS rules, insurance policy shifts, and ICD code changes (including ICD-11). Your eligibility scores and panel design never go stale as regulations evolve.
The Operational Shift: You never waste time chasing ineligible patients. Every enrollment minute is directed at a clinically appropriate, reimbursable candidate.
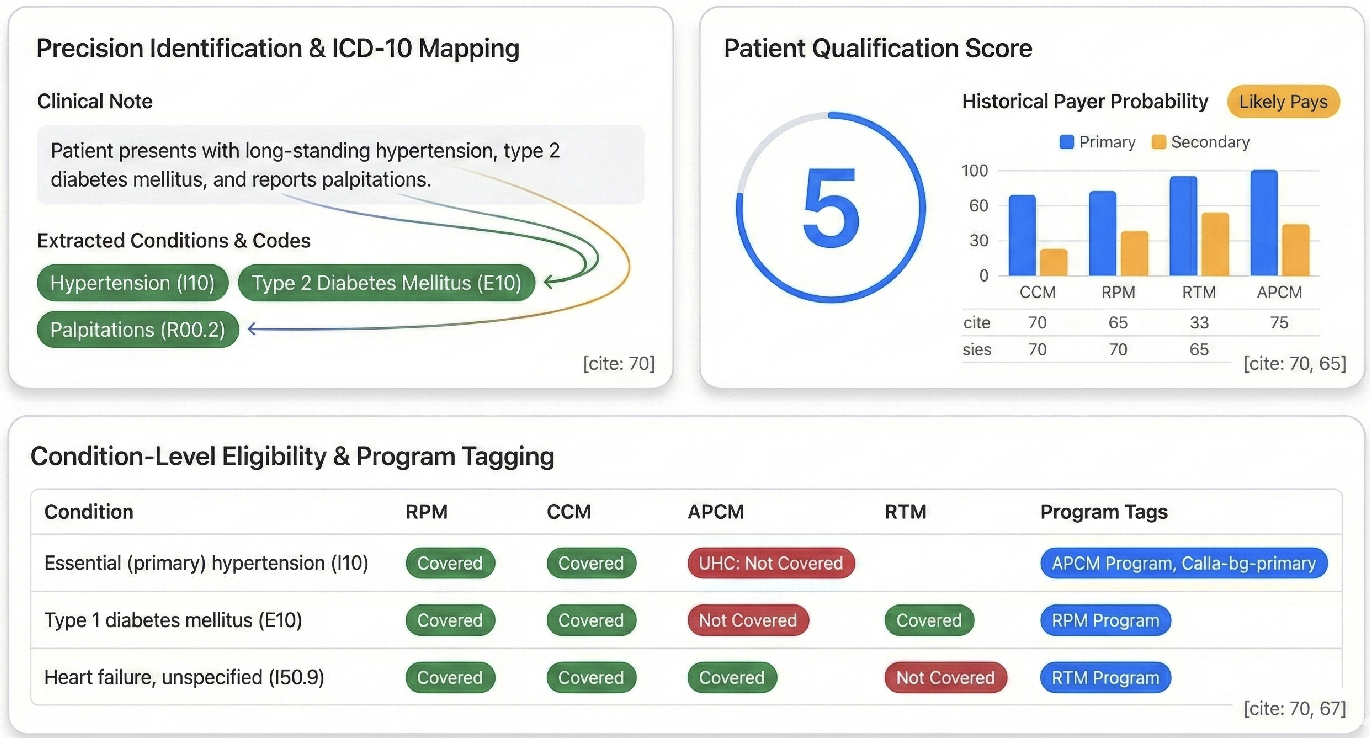
The 1–5 Score consolidates clinical data and payer history into one number.
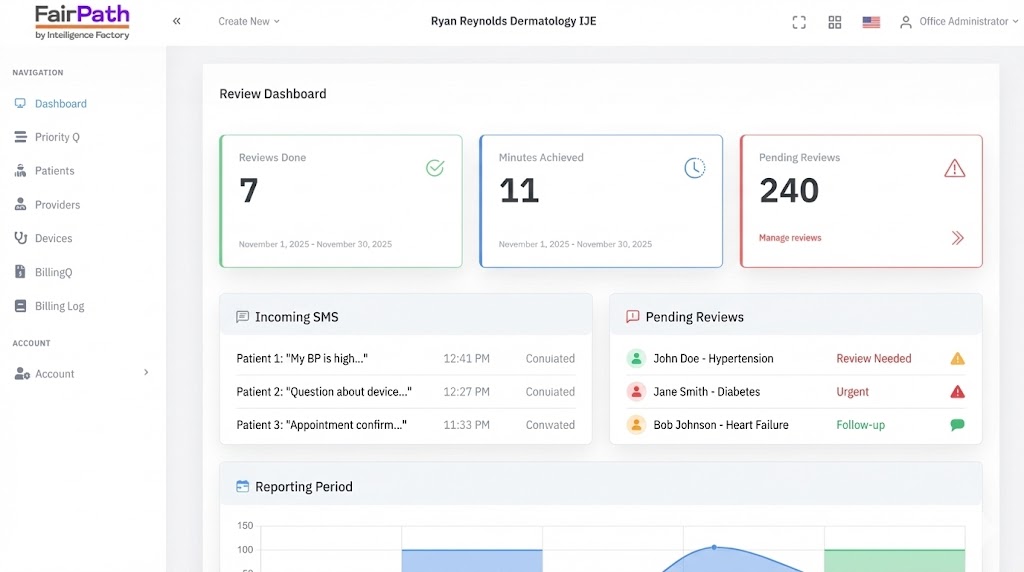
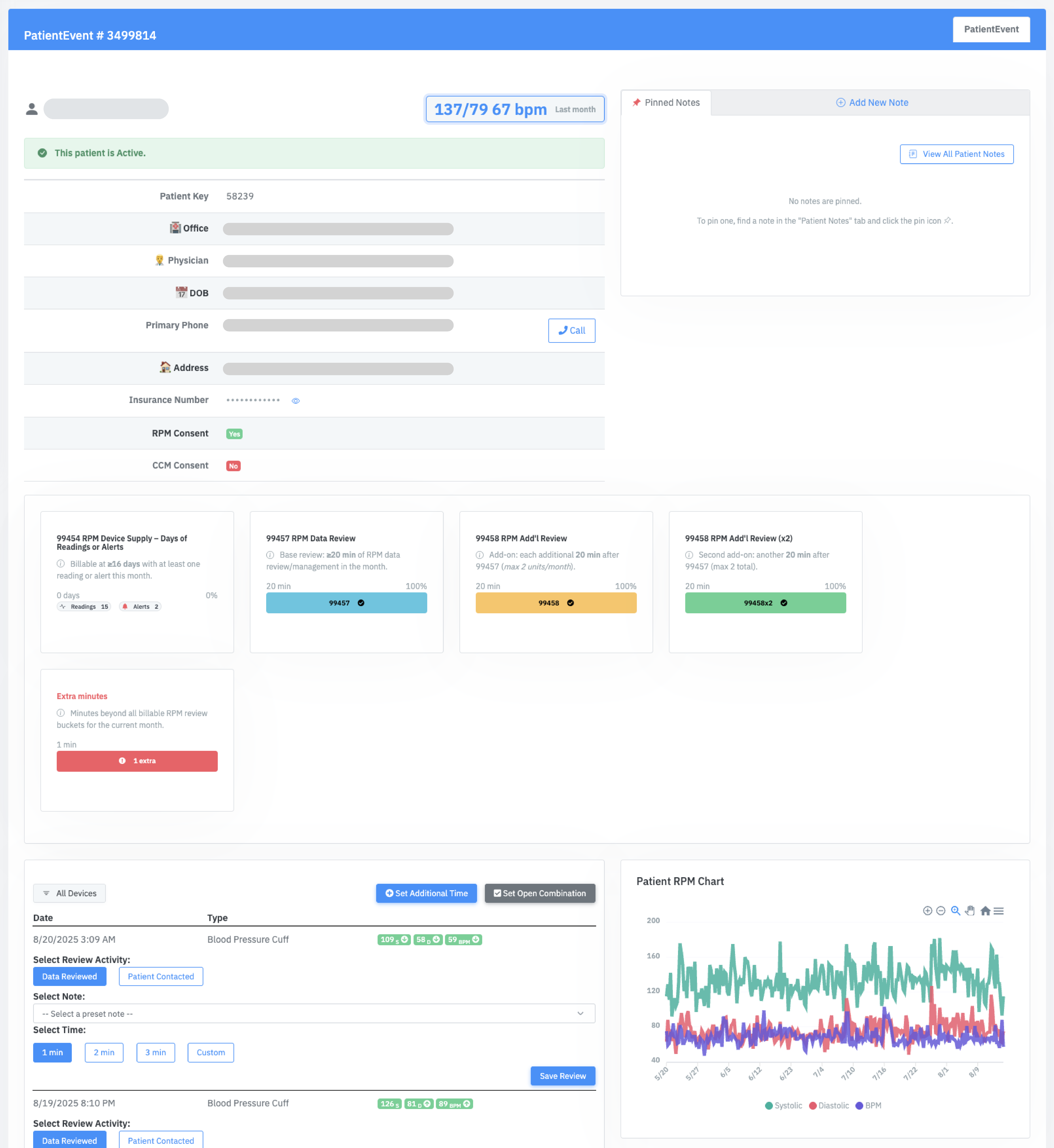
Daily Operational Command Center
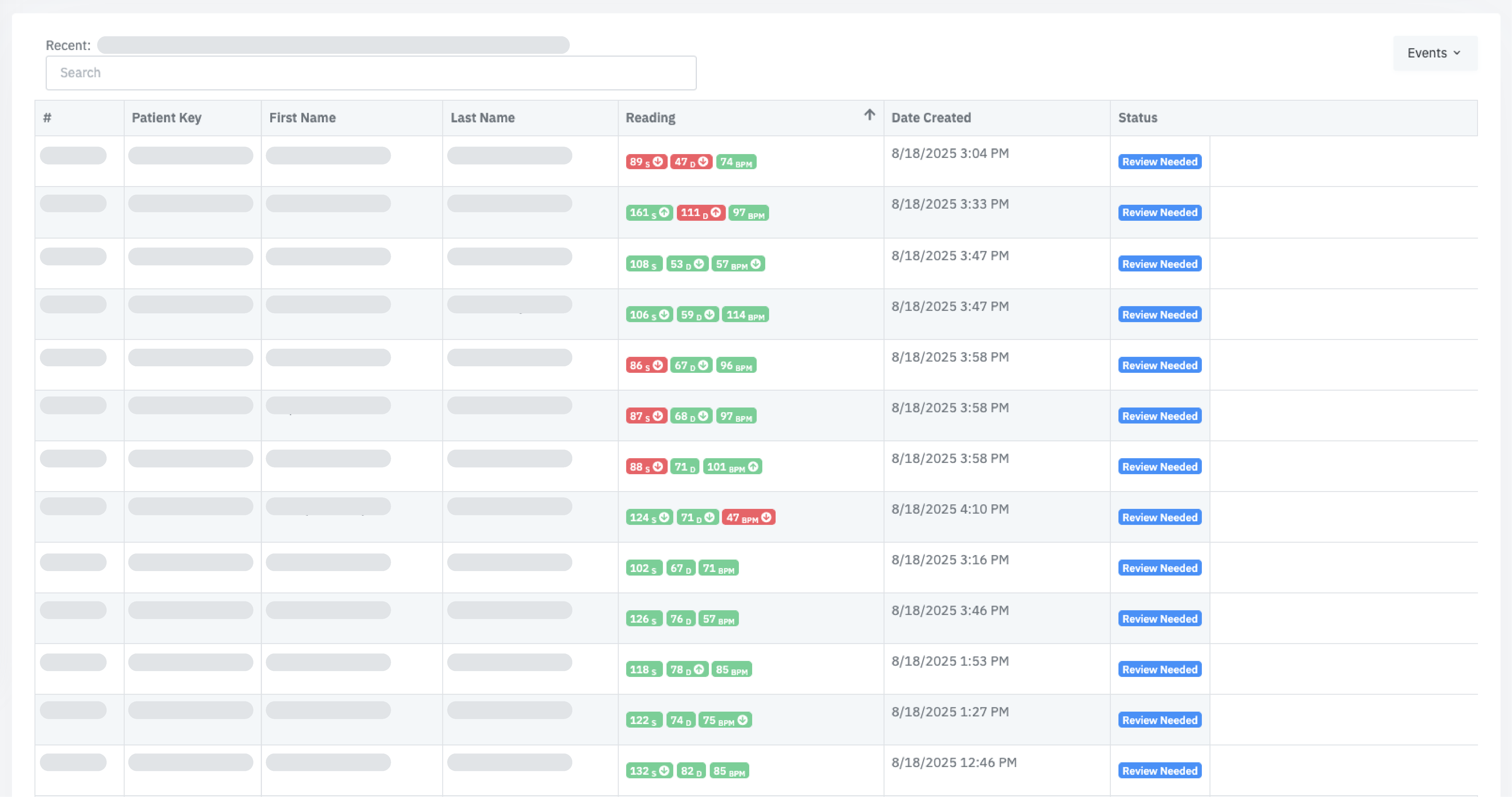
Your operations team lives in PriorityQ and ReviewQ—consolidated queues that sort work by urgency, clinical risk, and code completion. Instead of reviewing every reading, your staff works from a single queue of exceptions: critical vitals, worsening trends, and “no data” patterns. The same interface works for 50 or 5,000 patients; only the queue length changes, with Amy (AI) handling routine nudges and troubleshooting in the background.
Unified Queues
Consolidates new readings, APCM service tasks, “Device Problem” events, and exception alerts into one prioritized list so every click advances both patient outcomes and billing progress.
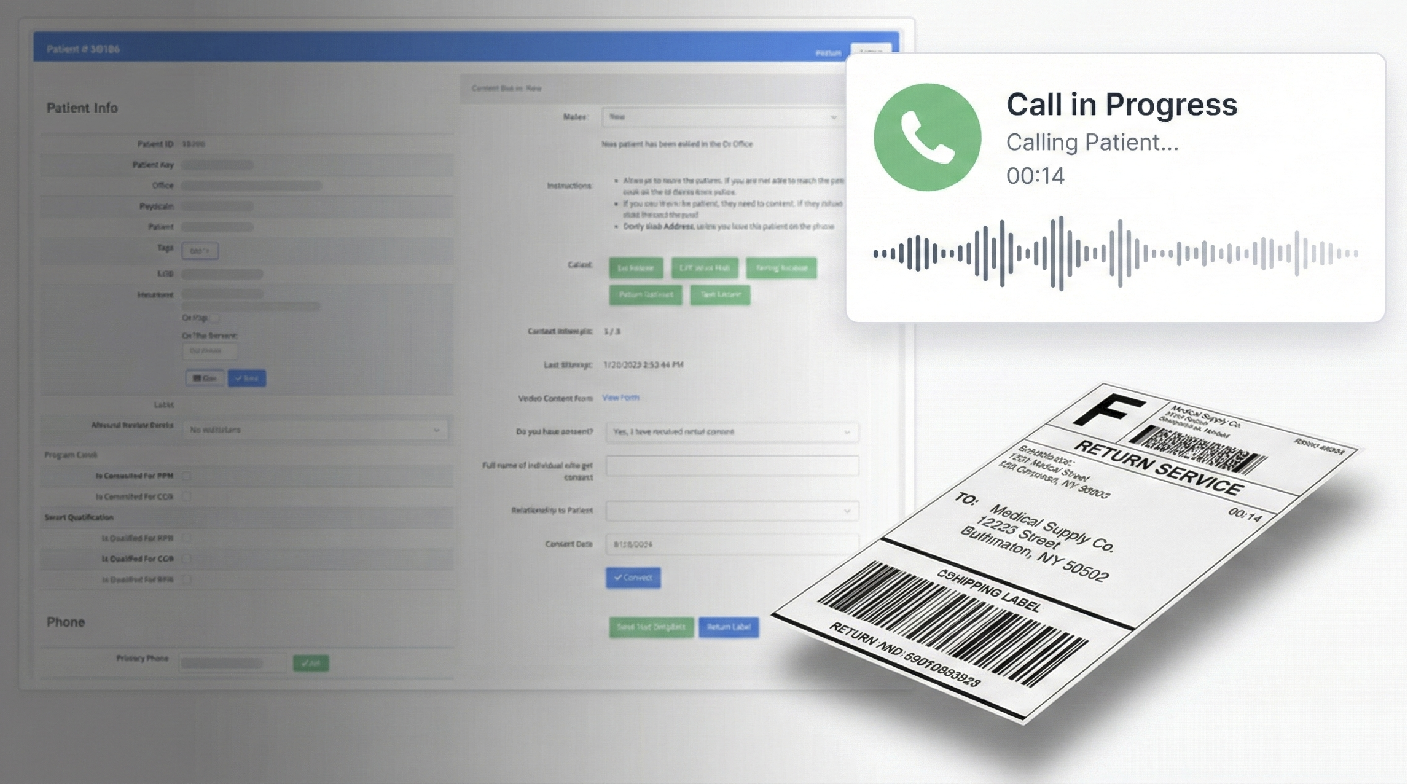
Integrated Comms
Calls and texts are initiated from the queue. Every interaction is timestamped and attached to the patient record, feeding BillingQ and your audit trail automatically.
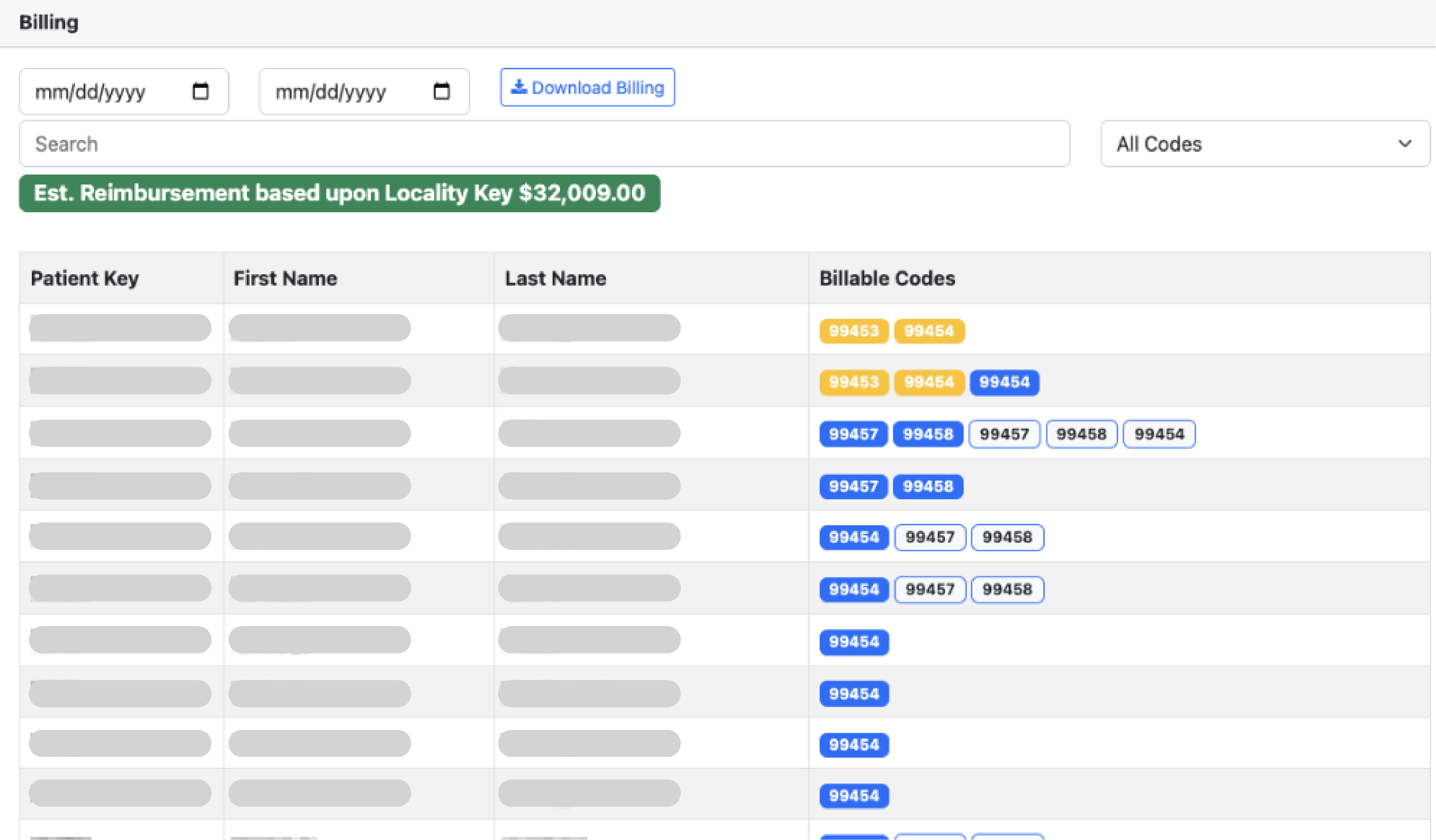
BillingQ: The Pre-Flight Check
Make “Compliance-as-Code” real. BillingQ treats compliance as a systems problem, not a training problem—encoding the rules so risky claims never make it to your billing team.
-
Cross-Program Rules Engine:
Understands how RPM, RTM, CCM, and APCM interact. Bundles APCM services correctly and enforces RPM’s structural rules (like 16 days of data) before a period is ever marked for billing review.
-
Embedded Regulatory Mapping:
OIG red flags and MAC guidance are encoded directly into BillingQ. If a patient hasn’t met thresholds or components, the claim is flagged and prevented from appearing in the “ready for billing review” list by your configured rules.
-
Code Stacking & Bundling:
Automatically flags conflicting codes (e.g., RPM + CCM overlaps) and ensures APCM bundles meet all service requirements before billing.
-
Automatic Time Tracking:
Every interaction—calls, reviews, messages—is timestamped and categorized automatically, aggregating time toward the correct codes without manual tallies.
Audit Defense:
Logs all readings, alerts, consents, and care-plan updates so you can answer OIG queries about “incomplete components”. No wasted motion—every action is tracked for reimbursement, and the system warns you if an activity won’t support a compliant claim, protecting both revenue and your license.