RPM Manual
The practical 2026 guide to device rules, day thresholds, management time, and audit defensibility for Remote Patient Monitoring.
Read the RPM Guide →We do not ask for PHI or raw claim files. Instead, we look at the same high-level signals CMS and OIG use: how far your charges sit above Medicare allowance, whether patients actually hit the 16-day rule, how many hours you bill, and whether required components show up together.
Every report follows a similar structure to our internal RPM Compliance & Optimization analyses-- personalized to your practice, codes, and current vendor or software stack.
We take your RPM/RTM billing and utilization patterns and map them against the exact red flags CMS and the OIG have already published--then show you how to fix what we find.
We compare your submitted charges for RPM codes to Medicare allowance and to national peers, highlighting where you look like normal practice and where you resemble the outliers OIG calls out for excessive charge levels and questionable patterns.
We assess how often your patients actually hit the 16-day requirement for 99454 and similar codes, identify patient segments that consistently fall short, and quantify the clinical and billing risk tied to insufficient device utilization.
We look for implausible volumes of management time (99457/99458) and for enrollees who are missing required elements--onboarding, device, or review--mirroring the OIG’s 2024 RPM findings on abusive billing and incomplete services.
Your report is built from the same kinds of aggregate data CMS and the OIG use: not charts in a sales deck, but the hard numbers behind your RPM program.
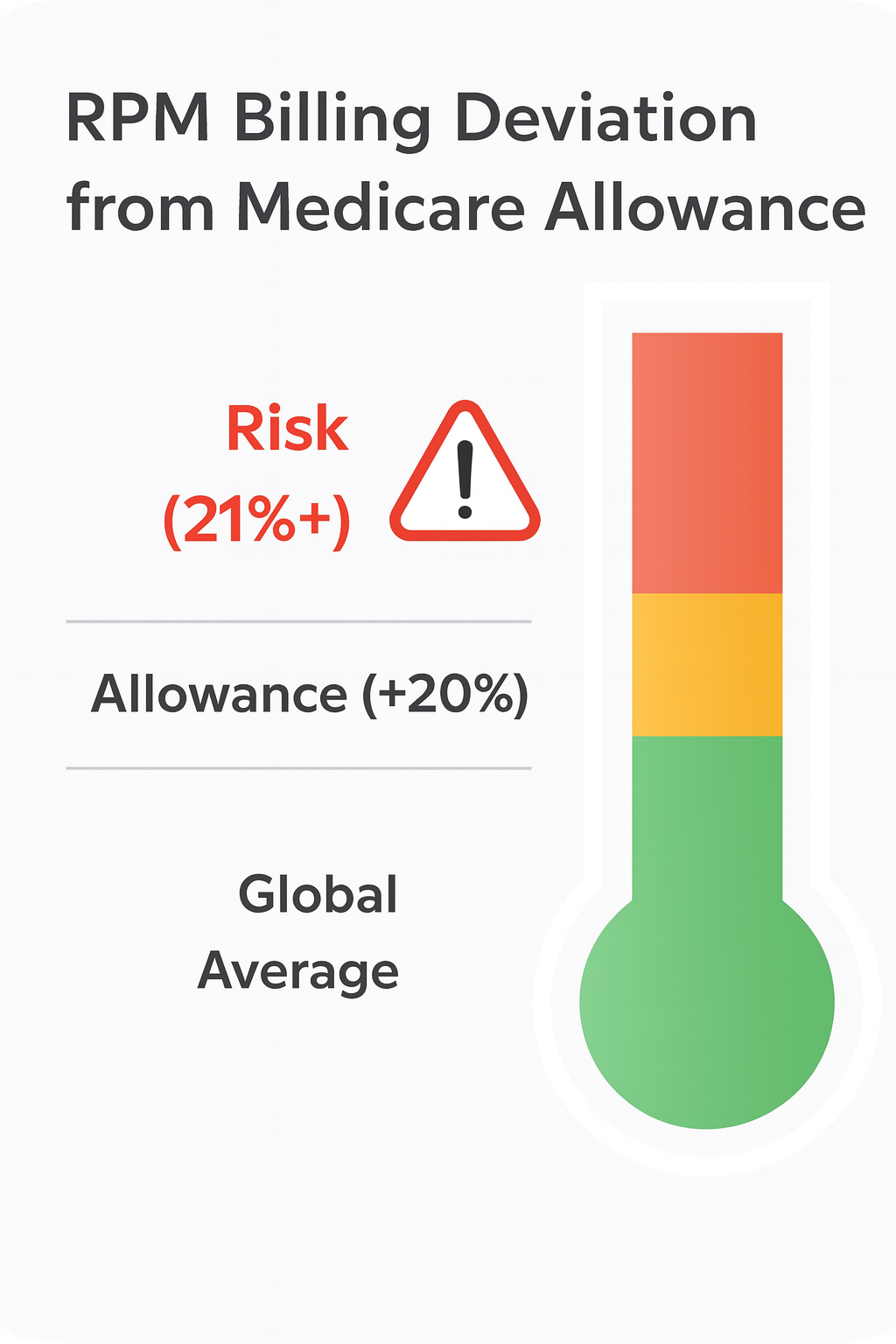
One example from the report: a simple indicator showing how your average RPM charge levels compare to Medicare allowance, global averages, and the risk zone where regulators start asking questions.
The report doesn’t just tell you what’s risky--it shows how FairPath’s Compliance-as-Code engine can neutralize those risks while improving revenue stability.
| Risk Area | What We Often See Today | What FairPath Does Instead |
|---|---|---|
| Charge Levels | RPM charges 50–200% above Medicare allowance, tuned to vendor revenue and commercial contracts, with no formal guardrails. | Benchmarking against allowance and national patterns; per-code charge limits and alerts prevent obviously risky charge behavior. |
| Device Utilization | 99454 billed month after month while many patients fall short of the 16-day rule and engagement is managed ad-hoc. | Automated day-counter, reminders, and risk flags for patients at risk of missing 16 days--plus documentation to prove who was contacted when. |
| Management Minutes | High volumes of 99457/99458 with little evidence of distinct, documented work or clear separation from CCM/APCM minutes. | Program-aware timers and coding logic that allocate minutes correctly across RPM, CCM, APCM, and RTM and flag implausible totals. |
| Missing Components | Enrollees with device or management codes but no clear record of onboarding, consent, or qualifying visits. | Structured enrollment and eligibility workflows that enforce required steps before billing and keep a clean audit trail for every patient. |
100% Confidential
No PHI Required
HIPAA-Aligned Infrastructure
No. We work from the same aggregate patterns CMS and the OIG use: charge levels, code usage, utilization per beneficiary, and total hours. We do not request patient names, DOBs, or other PHI for this assessment, and we can work from simple exports or summary data you already have.
This isn’t a denial score. It’s an OIG pattern-match score: how many of your signals line up with the RPM fraud profile OIG has already published. Your report shows exactly which red flags you’re lighting up—and how to shut them off.
You can take the findings back to your team or existing vendor, or you can ask us to help implement changes inside FairPath. There is no obligation to switch platforms--the report is designed to give you clarity first, then options.
We’ll build a tailored RPM Fraud Risk & Optimization Report using the same patterns CMS and the OIG watch--then walk you through it in plain language.
FairPath is built on operational work, not theory. We publish the playbooks and checklists we use to keep programs compliant and profitable. Use them whether you run FairPath or not.
Browse the Expert Library →The practical 2026 guide to device rules, day thresholds, management time, and audit defensibility for Remote Patient Monitoring.
Read the RPM Guide →How to run Remote Therapeutic Monitoring for MSK, respiratory, and CBT workflows with the correct 9897x and 9898x rules.
Read the RTM Guide →Calendar-month operations for CCM: consent, initiating visit, care plan requirements, time counting, and concurrency rules.
Read the CCM Guide →The operator blueprint for Advanced Primary Care Management: eligibility, G0556–G0558 tiers, and monthly execution.
Read the APCM Playbook →